
Can we design Ecological Interfaces that facilitate communication between physicians and patients with respect to understanding the rational underlying diagnoses and treatment decisions? Can we help both physicians and patients to understand how a wide range of factors impact health risks?
More than 10 years ago, Tim McEwen decided to do his dissertation with me on developing an Ecological Interface for the healthcare domain. He identified cardiovascular health as a reasonable candidate and he completed his dissertation in 2012 on the Cardiovascular Display (CVD) which reverse engineered the Framingham Risk Model into a direct manipulation interface for visualizing the impact of various factors on cardiovascular risk. After completing his degree, he took a job in the healthcare field and the expectation was that this would be an opportunity to develop his interface into a commercial product. However, things didn't work out the way we planned and the ideas languished for a few years, till in spring of 2017 I joined Mile Two and shared the ideas with the Mile Two Team.

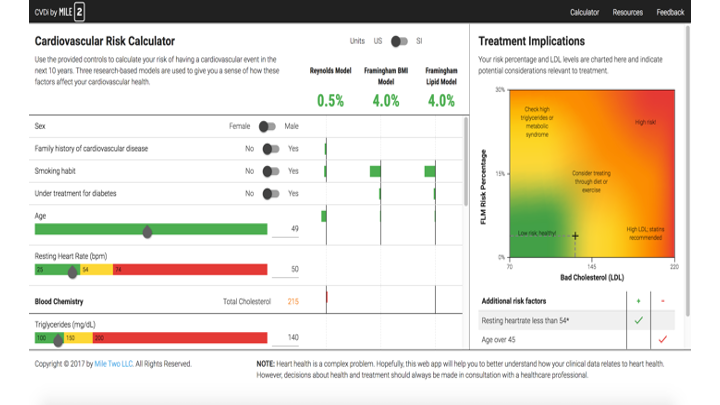
The CVD Interface developed for McEwen's dissertation (2012)
The Mile Two team immediately saw the possibilities for this interface, but laughed at our graphics and code. This led to the next generation interface - with a greatly improved interface that allowed us to add two more risk models (Reynolds, Framingham BMI) and that provided a direct comparison of the three models. The inclusion of multiple models was consistent with previous work I had been involved with related to Modeling to Generate Alternatives (MGA) (Brill, Flach, Hopkins & Ranjithan, 1990)*.
The hypothesis underlying MGA was that joint cognitive systems that included humans and automated decision tools would be more effective if the automated decisions systems were used to provide a range of different satisfying solutions, rather than a single 'optimal' solution. The central assumption is that computational models rarely take into account all the important factors for natural complex situations - so that an optimal solution to a model is rarely an optimal solution to the actual problem. Thus, the hypothesis is that in choosing among a few different solutions that satisfied the model - humans would be more likely to avoid fixating on a single or narrow range of solutions and would be more likely to take into account factors not considered in the model. In essence, the idea was to use the model solutions as seeds to stimulated human problem solving, rather than as 'answers' to displace human problem solving.
In essence, the idea was to use the model solutions as seeds to stimulated human problem solving, rather than as 'answers' to displace human problem solving.
So, the CVDi interface was designed to reduce the tendency for physicians to blindly apply a single risk model and to hopefully lead them to think more broadly about the situation of a specific patient. We also hoped that the graphical interface would help support a conversation between the patients and physicians - so that the patients could better understand the logic underlying treatment choices, and in turn they would be more likely to comply. For example, the physician might be able to show through direct manipulation the impact of a particular variable like smoking or LDL cholesterol on the likelihood of an adverse cardiac event. The new CVDi interface was presented at the HFES in Healthcare conference in 2018. After the presentation, we were approached by Asymmetric about the possibility that we might collaborate to create an app for the Cerner App Challenge.
The CVDi interface developed at Mile Two.
Asymmetric had extensive experience with the FHIR api, which was becoming a standard for accessing information from digital healthcare records. This would allow a patient's data to be directly accessed from their digital health record - rather than having the data entered manually on our interface. The result of that collaboration was the Cardiac Consultant which was awarded third place in the 2019 Cerner App Challenge. In designing the interface for the Cardiac Consultant we decided to show the risk estimates for each different model, but to see the contributions for each individual component/variable, the physician would need to select a specific model. The motivation was to reduce the overall complexity of the representation. The full range of risk values from the models was presented, but the physician had to choose a single model in order to see the details of the individual variable weights. These could be compared sequentially, but were not displayed simultaneously as with the CVDi.
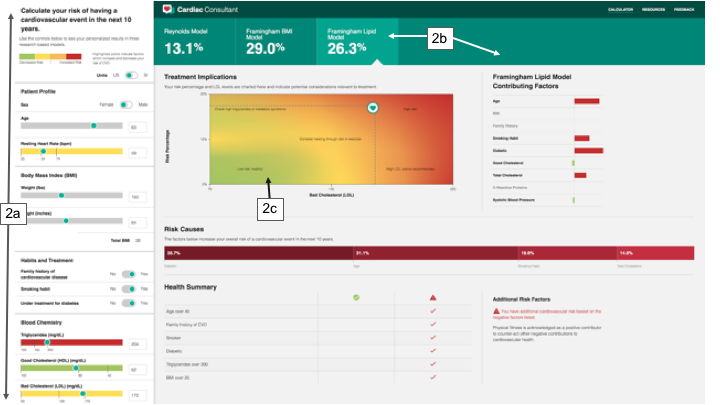
The Cardiac Consultant developed in collaboration with Asymmetric.
After the collaboration with Asymmetric, Mile Two continued development of the concept with the specific goal of designing a version that could be integrated into a patient portal. The goal was to add more explanations and we also added a diabetes risk model, since there is a very close relation between diabetes and cardiac risk. This iteration was the Clinical Consultant.

The Clinical Consultant developed by the Mile Two team.
Despite continuous development and refinement, we have not been able to get traction in the Healthcare Industry. Currently all three apps can be accessed online for manual entry of health data to estimate risks, but they have not been interfaced to any patient databases.
Below you can find links to the video that describes the Cardiac Consultant that was submitted for the Cerner App Challenge. Also, links to the CVDi, the Cardiac Consultant, and the Clinical Consultant are posted below. These are all live apps that will allow you to enter data to assess your own health or to explore hypotheses about how various factors impact health. We welcome feedback and suggestions for how this work might be implemented in existing digital healthcares systems.
YouTube Video: https://www.youtube.com/watch?v=eucU7cY51w4
Cardiac Consultant: https://cardiac-consultant-demo.asymmetrik.com/
CVDi: https://mile-two.gitlab.io/CVDI/
Clinical Consultant (in development): https://cvdi.edge.mile-two.com/metabolic
*Brill, E.D. Jr., Flach, J.M., Hopkins, L.D., & Ranjithan, S. (1990). MGA: A decision support system for complex, incompletely defined problems. IEEE Transactions on Systems, Man, and Cybernetics, 20(4), 745-757.
Other relevant references:
Flach, J., Reynolds, P., Duryee, L., Young, B. & Graley, J. (2019). Digital Healthcare: Moving beyond the data input/output problem toward enhancing clinical judgment. Proceedings of the International Symposium on Human Factors and Ergonomics in Healthcare, 8(1), 57-61. Chicago, IL (March 25-27).
Flach, J.M., Schanely, P., Kuenneke, L., Chidoro, B., Mubaslat, J. & Howard, B. (2018) Electronic health records and evidence-based practice: Solving the little data problem. Proceedings of the International Symposium on Human Factors and Ergonomics in Health Care, 7(1), 30-35.
Flach, J.M., Reynolds, P., Cao, C. & Saffell, T. (2017). Engineering representation to support evidence based practice. Proceedings of the International Symposium on Human Factors and Ergonomics in Healthcare, 6(1), 66-73. New Orleans, LA (March 5-8).
McEwen, T., Flach, J.M. & Elder, N. (2014). Interfaces to medical information systems: Supporting evidence-based practice. IEEE: Systems, Man, & Cybernetics Annual Meeting, 341-346. San Diego, CA. (Oct 5-8).
